Ophthalmic Artery
Origin
The ophthalmic artery is a branch of the cerebral part of the internal carotid artery, given off medial to the anterior clinoid process close to the optic canal
Course and Relations
1. The artery enters the orbit through the optic canal, lying inferolateral to the optic nerve.
Both the artery and nerve lie in a common dural sheath.
2. In the orbit, the artery pierces the dura mater, ascends over the lateral side of the optic nerve, and
crosses above the nerve from lateral to medial side along with the nasociliary nerve.
It then runs forwards along the medial wall of the orbit between the superior oblique and the medial rectus muscles, and parallel to the nasociliary nerve.
3. It terminates near the medial angle of the eye by dividing into the supratrochlear and dorsal nasal branches
Branches
While still within the dural sheath, the ophthalmic artery gives off the central artery of the retina.
After piercing the dura mater, it gives off a large lacrimal branch that runs along the lateral wall of the orbit.
The main artery runs towards the medial wall of the orbit giving off a number of branches.
The central artery of retina is the first and most important branch of the ophthalmic artery.
It first lies below the optic nerve.
It pierces the dural sheath of the nerve and runs forwards for a short distance between these two.
It then enters the substance of the nerve and runs forwards in its centre to reach the optic disc
Here it divides into branches that supply the retina
The central artery of the retina is an end artery.
It does not have effective anastomoses with other arteries.
Occlusion of the artery results in blindness.
The intraocular part of the artery can be seen, in the living, through an ophthalmoscope.
- It accompanies the ophthalmic artery.
- It lies above the optic nerve.
- It receives tributaries corresponding to the branches of the artery,
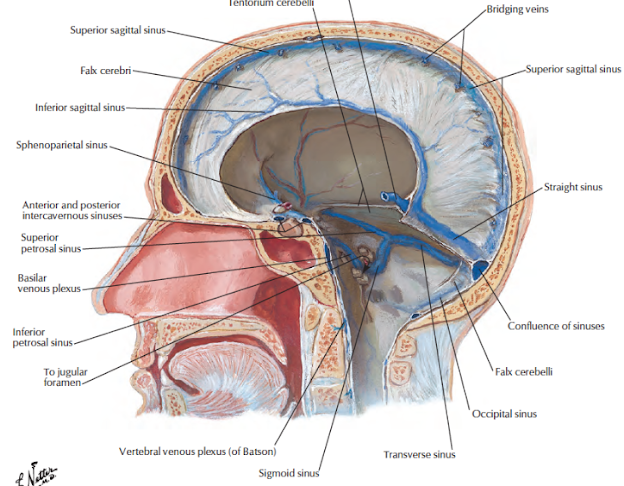
- passes through the superior orbital fissure, and drains into the cavernous sinus.
- It communicates anteriorly with the supraorbital and angular veins