Longus colli (cervicis)
Origin
a. The upper oblique part is from the anterior tubercles of the transverse processes of cervical vertebrae 3, 4, 5
b. Lower oblique part is from bodies of upper 2-3 thoracic vertebrae
c. Middle vertical part is from bodies of upper 3 thoracic and lower 3 cervical vertebrae
lnsertion
a. Upper oblique part is into the anterior tubercle of the atlas
b. Lower oblique part is into the anterior tubercles of the transverse processes of 5th and 6th cervical vertebrae
c. Middle vertical part is into bodies of 1, 2,3,4 cervical vertebrae
Nerve supply
Ventral rami of nerves C3-C8
Actions
a. Flexes the neck
b. Oblique parts flex the neck laterally
c. Lower oblique part rotates the neck to the opposite side
Longus capitis
Origin
Anterior tubercles of transverse processes of cervical 3-6 vertebrae
Insertion
lnferior surface of basilar part of occipital bone
Nerve Supply
Ventral rami of nerves C1-C3
Action
Flexes the head
Rectus capitis anterior
Origin
Anterior surface of lateral mass of atlas in front of the occipital condyle
Insertion
Basilar part of the occipital bone
Nerve Supply
Ventral ramus of nerve C1
Action
Flexes the head
Rectus capitis lateralis
Origin
Upper surface of transverse process of atlas
Insertion
lnferior surface of jugular process of the occipital bone
Nerve Supply
Ventral rami of C2, C1 nerves ,
Action
Flexes the head laterally
SCALENOVERTEBRAL TRIANGLE
The triangle is present at the root of the neck.
Boundaries
Medial: Lower oblique part of longus colli
Lateral: Scalenus anterior
Apex: Transverse process of cervical C6 vertebra
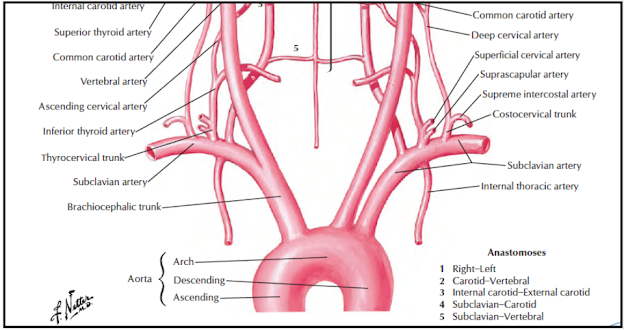
Base: 1st part of subclavian artery
Posterior wall: Transverse process of C7, Ventral ramus of C8 nerve, neck of 1st rib and cupola of
pleurae
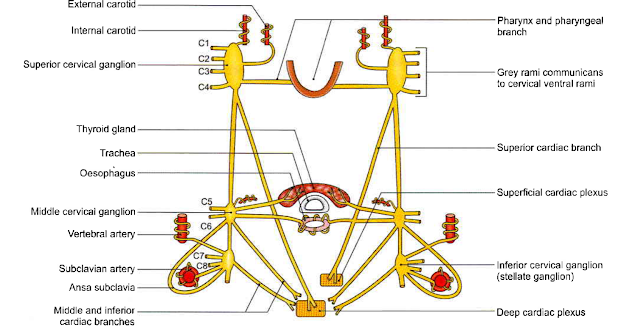
Contents: 1st part of vertebral artery, cervical part
of sympathetic trunk
Watch the lectures on YouTube: