The deep fascia of the neck is condensed to form the following layers:
1. Investing layer
2. Pretracheal layer
3. Prevertebral layer
4. Carotid sheath
5. Buccopharyngeal fascia
6.Pharyngobasilar fascia.
INVESTING LAYER
It lies deep to the platysma,
surrounds the neck like a collar.
It forms the roof of the posterior triangle of the neck
Attachments
Superiorly :
a. External occipital protuberance
b. Superior nuchal line
c. Mastoid process
d. External acoustic meatus
e. Base of the mandible.
Between the angle of the mandible and the mastoid
process/ the fascia splits to enclose the parotid gland
The superficial lamina named as parotid fascia
is thick and dense, and is attached to the zygomatic arch.
The deep lamina is thin and is attached to the styloid
process, the mandible and the tympanic plate.
Between the styloid process and the angle of the mandible,
the deep lamina is thick and forms the stylomandibular
ligament which separates the parotid gland from the
submandibular gland, and is pierced by the external carotid
artery.
At the base of mandible, it encloses submandibular gland. The superficial lamina is attached to lower border of body of
mandible and deep lamina to the mylohyoid line.
Inferiorly:
a. Spine of scapula,
b. Acromion process
c. Clavicle, and
d. Manubrium.
The fascia splits to enclose the suprasternal and supraclavicular spaces,
Other Features:
1. The investing layer of deep cervical fascia splits to enclose:
a. Muscles: Trapezius and sternocleidomastoid.
b. Salivary glands: Parotid and submandibular.
c. Spaces: Suprasternal and supraclavicular.
2 It also forms pulleys to bind the tendons of the digastric and omohyoid muscles.
3 Forms roof of anterior and posterior triangles.
4 Forms stylomandibular ligament and parotidomasseteric fasciae.
Clinical Anatomy
- Parotid swellings are very painful due to the unyielding nature of parotid fascia.
- While excising the submandibular salivary gland, the external carotid artery should be secured before dividing it, otherwise it may retract through the stylomandibular ligament and cause serious bleeding.
- Division of the external jugular vein in the supraclavicular space may cause air embolism and consequent death because the cut ends of the vein are prevented from retraction and closure by the fascia, attached firmly to the vein
PRETRACHEAL FASCIA
The importance of this fascia is that it encloses and suspends the thyroid gland and forms its false capsule Attachments:
Superiorly
1. Hyoid bone in the median plane.
2. Oblique line of thyroid cartilage laterally.
3. Cricoid cartilage-more laterally.
Inferiorly
Below the thyroid gland, it encloses the
inferior thyroid veins, passes behind the
brachiocephalic veins, and finally blends with
the arch of the aorta and fibrous pericardium.
On either side
It forms the front of the carotid sheath, and
fuses with the fascia deep to the
sternocleidomastoid
Other Features
- The posterior layer of the thyroid capsule is thick.
-
On either side, it forms a suspensory ligament for the thyroid gland known as ligament of
Berry
- The ligaments are attached chiefly to the cricoid cartilage, and may extend to the thyroid cartilage.
- They support the thyroid gland, and do not let it sink into the mediastinum.
- The capsule of the thyroid is very weak along the posterior borders of the lateral lobes.
- The fascia provides a slippery surface for free movements of the trachea during swallowing.
Clinical anatomy
Neck infections in front of the pretracheal fascia may bulge in the suprasternal area or extend down into the anterior mediastinum.
The thyroid gland and all thyroid swellings move with deglutition because the thyroid is attached to cartilages of the larynx by the suspensory ligaments of Berry.
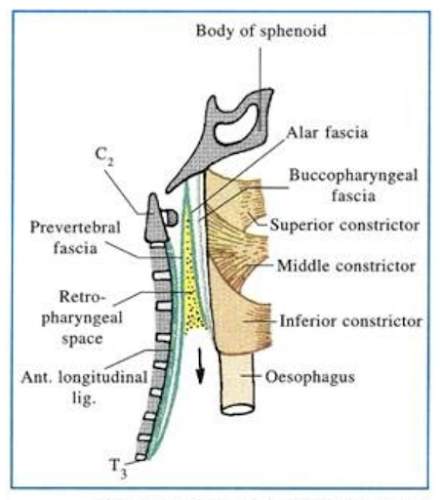
PREVERTEBRAL FASCIA
It lies in front of the prevertebral muscles, and forms
the floor of the posterior triangle of the neck
Attachments and Relations
Superiorly
It is attached to the base of the skull.
Inferiorly
It extends into the superior mediastinum where it splits into anterior and posterior layers.
Anterior layer / alar fascia blends with
buccopharyngeal fascia and
posterior layer is attached to the anterior
longitudinal ligament and to the body of the fourth
thoracic vertebra.
Anteriorly
It is separated from the pharynx and
buccopharyngeal
fascia by the retropharyngeal space containing loose
areolar tissue.
Posteriorly
It is lies deep to the trapezius and is attached to
fascia of sternocleidomastoid muscle.
Other Features
- The cervical and brachial plexuses lie behind the prevertebral fascia.
- The fascia is pierced by the four cutaneous branches of the cervical plexus
- As the trunks of the brachial plexus, and the subclavian artery, pass laterally through the interval between the scalenus anterior and the scalenus medius, they carry with them a covering of the prevertebral fascia known as the axillary sheath which extends into the axilla.
- The subclavian and axillary veins lie outside the sheath and as a result they can dilate during increased venous return from the limb.
- Fascia provides a fixed base for the movements of the pharynx, the oesophagus and the carotid sheaths during movements of the neck and during swallowing.
Neck infections behind the prevertebral fascia arise usually from tuberculosis of the cervical vertebrae or cervical caries.
Pus produced as a result may extend in various directions.
It may pass forwards forming a chronic retropharyngeal abscess which may form a bulging in the posterior wall of the pharynx, in the median plane.
The pus may extend laterally through the axillary sheath and point in the posterior triangle, or in the lateral wall of the axilla.
It may extend downwards into the superior mediastinum where its descent is limited by fusion of the prevertebral fascia to the fourth thoracic vertebra.
Neck infections in front of the prevertebral fascia in the retropharyngeal space usually arise from suppuration; i.e. formation of pus in the retropharyngeal lymph nodes.
The pus forms an acute retropharyngeal abscess which bulges forwards in the paramedian position due to fusion of the buccopharyngeal fascia to the prevertebral fascia in the median plane,
The infection may extend down through the superior mediastinum into the posterior mediastinum
CAROTID SHEATH
It is a condensation of the fibroareolar tissue around the main vessels of the neck.
It is formed on anterior aspect by pretracheal fascia and on posterior aspect by prevertebral fascia.
The contents are the common or internal carotid arteries, internal jugular vein and the vagus nerve.
It is thin over the vein.
In the upper part of sheath there are IX,XI, XII nerves also.
These nerves pierce along with external carotid artery.
Relations
1 The ansa cervicalis lies embedded in the anterior
wall of the carotid sheath.
2 The cervical sympathetic chain lies behind the
sheath, plastered to the prevertebral fascia.
3 The sheath is overlapped by the anterior border of
the sternocleidomastoid, and is fused to the layers
of the deep cervical fascia.
BUCCOPHARYNGEAL FASCIA
This fascia covers the superior constrictor
muscle externally and
extends on to the superficial aspect of
the buccinator muscle.
PHARYNGOBASILAR FASCIA
- This fascia is especially thickened between the upper border of superior constrictor muscle and the base of the skull.
- It lies deep to the pharyngeal muscles








No comments:
Post a Comment