- The parotid is the largest of the salivary glands.
- It weighs about 15 g.
- It is situated below the external acoustic meatus, between the ramus of the mandible and the sternocleidomastoid.
- The gland overlaps these structures.
- Anteriorly, the gland also overlaps the masseter muscle.
- A part of this forward extension is often detached, and is known as the accessory parotid, and it lies between the zygomatic arch and the parotid duct.
Capsule of Parotid Gland
- The investing layer of the deep cervical fascia forms
a capsule for the gland.
- The fascia splits (between the angle of the mandible and the mastoid process) to enclose the gland.
- The superficial lamina, thick and adherent to the
gland, is attached above to the zygomatic arch.
- The deep lamina is thin and is attached to the styloid process, the angle and posterior border of the ramus of the mandible and the tympanic plate.
- A portion of the deep lamina, extending between the styloid process and the mandible, is thickened to form the stylomandibular ligament which separates the parotid gland from the submandibular salivary gland.
- The ligament is pierced by the external carotid artery
Clinical Anatomy
- Parotid swellings are very painful due to the unyielding nature of the parotid fascia.
- Mumps is an infectious disease of the salivary glands (usually the parotid) caused by a specific virus,
- Viral parotitis or mumps characteristically does not suppurate. Its complications are orchitis and pancreatitis
External Features
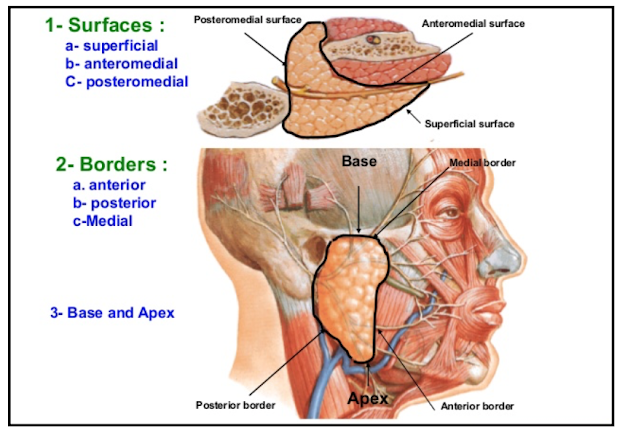
The gland resembles a three sided pyramid.
The apex of the pyramid is directed downwards
The gland has four surfaces:
- a. Superior (base of the pyramid)
- b. Superficial
- c. Anteromedial
- d. Posteromedial.
- a. Anterior
- b. Posterior
- c. Medial/pharyngeal
Relations
- The apex overlaps the posterior belly of the digastric
and the adjoining part of the carotid triangle.
- The cervical branch of the facial nerve and the two divisions of the retromandibular vein emerge near the apex.
Surfaces
The superior surface or base forms the
upper end of the gland which is small and
concave.
It is related to:
- a. The cartilaginous part of the external acoustic meatus.
- b. The posterior surface of the temporomandibular joint.
- c. The superficial temporal vessels.
- d. The auriculotemporal nerve
The superficial surface is the largest of the
four surfaces.
It is covered with:
- a. Skin
- b. Superficial fascia containing the anterior branches of the great auricular nerve, the preauricular or superficial parotid lymph nodes and the posterior fibres of the platysma and risorius.
- c. The parotid fascia which is thick and adherent to the gland.
- d. A few deep parotid lymph nodes embedded in the gland
The anteromedial surface is grooved by the
posterior border of the ramus of the mandible.
It is related to:
- a. The masseter
- b. The lateral surface of the temporomandibular joint.
- c. The posterior border of the ramus of the mandible
- d. The medial pterygoid
- e. The emerging branches of the facial nerve.
The posteromedial surface is moulded to the mastoid and the styloid processes and the structures attached to them.
Thus it is related to:
- a. The mastoid process, with the sternocleidomastoid and the posterior belly of the digastric.
- b. The styloid process, with structures attached to it.
- c. The external carotid artery enters the gland through this surface and the internal carotid artery lies deep to the styloid process
Borders
- The anterior border separates the superficial
surface from the anteromedial surface.
- It extends from the anterior part of the superior surface to the apex.
The following structures emerge at this border:
- a. The parotid duct.
- b. Most of the terminal branches of the facial nerve.
- c. The transverse facial vessels. In addition, the accessory parotid gland lies on the parotid duct close to this border.
The posterior border separates the superficial surface from the posteromedial surface.
- It overlaps the sternocleidomastoid.
The medial edge or pharyngeal border
separates the anteromedial surface from the
posteromedial surface.
- It is related to the lateral wall of the pharynx
Structures within the parotid gland
From medial to the lateral side, these are as follows.
Arteries:
- The external carotid artery enters the gland through its posteromedial surface.
- The maxillary artery leaves the gland through its anteromedial surface.
- The superficial temporal artery gives transverse facial artery and emerges at the anterior part of the superior surface.
Veins:
- The retromandibular vein is formed within the gland by the union of the superficial temporal and maxillary veins.
- In the lower part of the gland, the vein divides into anterior and posterior divisions which emerge close to the apex (lower pole) of the gland.
Nerve:
- facial nerve exits from cranial cavity through stylomastoid foramen and enters the gland through the upper part of its posteromedial surface, and divides into its terminal branches within the gland.
- The branches leave the gland through its anteromedial surface, and appear on the surface at the anterior border.
- Facial nerve lies in relation to isthmus of the gland which separates large superficial part from small deep part of the gland.
Facial nerve divides into two branches
- a. Temporofacial: Divides into temporal and zygomatic branches.
- b. Cervicofacial: Divides into buccal, marginal mandibular and cervical branches.
- The various branches (5-6) of facial nerve radiate like a goose-foot from the curved anterior border of the parotid gland to supply the respective muscles of facial expression. This pattern of branching is called "pes anserinus".
Patey's faciovenous plane
The gland is composed of a large superficial and a small deep part the two being connected by an 'isthmus' around which facial nerve divides
Accessory processes of parotid gland
- Facial process - along parotid duct
- Pterygoid process - between mandibular
ramus and medial pterygoid.
- Glenoid process - between external acoustic meatus and temporomandibular joint
- Poststyloid process
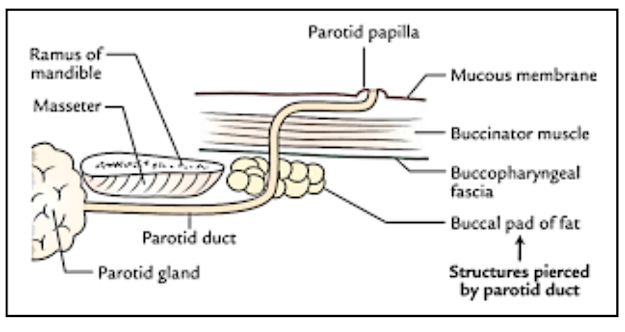
Parotid Duct / Stenson’s Duct
- It is thick walled and is about 5 cm long.
- It emerges from the middle of the anterior border of the gland
- It runs forwards and slightly downwards on the masseter. Here its relations are:
1. Accessory parotid gland.
2. The transverse facial vessels.
3. Upper buccal branch of the facial nerve.
Inferiorly
The lower buccal branch of the facial nerve.
At the anterior border of the masseter, the parotid
duct turns medially and pierces:
a. The buccal pad of fat.
b. The buccopharyngeal fascia.
c. The buccinator (obliquely).
Because of the oblique course of the duct
through the buccinator, inflation of the duct is
prevented during blowing.
The duct runs forwards for a short distance
between the buccinator and the oral mucosa.
Finally, the duct turns medially and opens into the vestibule of the mouth (gingivobuccal vestibule) opposite the crown of the upper second molar tooth
Clinical Anatomy
- Parotid abscess may be caused by spread of infection from the opening of parotid duct in
the mouth cavity.
- Parotidectomy is the removal of the parotid gland.
- After this operation, at times, there may be regeneration of the secretomotor fibres in the auriculotemporal nerve which join the great auricular nerve.
- This causes stimulation of the sweat glands and hyperaemia in the area of its distribution, thus producing redness and sweating in the area of skin supplied by the nerve.
- This clinical entity is called Frey Syndrome.
- Whenever, such a person chews there is increased sweating in the region supplied by auriculotemporal nerve.
- It is also called 'auriculotemporal syndrome'.
BIood Supply
- The parotid gland is supplied by the external carotid artery and its branches that arise within the gland.
- The veins drain into the external jugular vein and internal jugular vein.
Nerve Supply
- 1. Parasympathetic nerves are secretomotor They reach the gland through the auriculotemporal nerve.
- 2 Sympathetic nerves are vasomotor, and are derived from the plexus around the middle meningeal artery.
- 3 Sensory nerves to the gland come from the auriculotemporal nerve, but the parotid fascia is innervated by the sensory fibres of the great auricular nerve (C2, C3)
Lymphatic Drainage
Lymph drains first to the parotid nodes and from there to the upper deep cervical nodes.
DEVELOPMENT
The parotid gland is ectodermal in origin.
It develops from the buccal epithelium just lateral to the angle of mouth. The outgrowth branches repeatedly
to form the duct system and acini.
The mesoderm forms the intervening connective tissue septa.
Clinical Anatomy
- A parotid abscess is best drained by horizontal incision known as Hilton's method
below the angle of mandible
- During surgical removal of the parotid gland or parotidectomy the facial nerve is preserved by removing the gland in two parts, superficial and deep separately,
- The plane of cleavage is defined by tracing the nerve from behind forwards.
- Mixed parotid tumour is a slow growing lobulated painless tumour without any involvement of the facial nerve.
- Malignant change of such a tumour is indicated by pain, rapid growth, fixity with hardness, involvement of the facial nerve, and enlargement of cervical lymph nodes.
- The parotid calculi may get formed within the parotid gland or in its Stenson's duct.
- These can be located by injecting a radiopaque dye through its opening in the vestibule of the mouth. The procedure is called 'Sialogram'.
- The duct can be examined by a spatula or bidigital examination.
















No comments:
Post a Comment