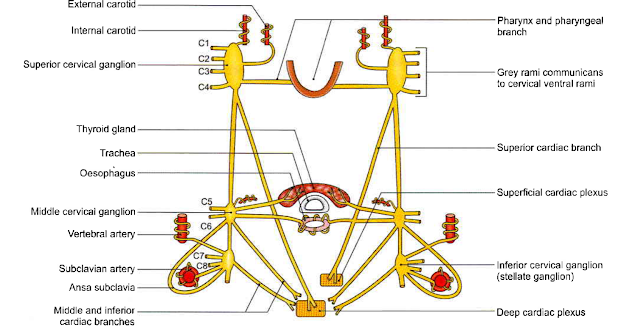
- The cervical parts of the right and left sympathetic trunks
- are situated one on each side of the cervical part of the vertebral column,
- behind the carotid sheath
- in front of the prevertebral fascia.
FORMATION
- There are no white rami communicans in the neck
- this part of the trunk is formed by fibres which emerge from segments T1 to T4 of the spinal cord, and
- then ascend into the neck.
- Grey rami communicans (i.e. outgoing roots) are present.
RELATIONS
Anterior
a. Internal carotid artery
b. Common carotid artery
c. Carotid sheath
d. Inferior thyroid artery.
Posterior
a. Prevertebral fascia
b. Longus capitis and cervicis muscles
c. Transverse processes of the lower six cervical vertebrae.
Superior Cervical Ganglion
Size & Shape
This is the largest of the three ganglia.
It is spindle shaped, and about 2.5 cm long.
Situation & Formation
It lies just below the skull,
opposite the second and third cervical vertebrae, behind the carotid sheath and in front of the prevertebral fascia (longus capitis).
It is formed by fusion of the upper 4 cervical ganglia.
Communication:
With cranial nerves IX, X and XII,
and with the external and recurrent laryngeal nerves
Branches
1. Grey rami communicans pass to the ventral rami of upper four cervical nerves.
2. The internal carotid nerve arises from the upper end of the ganglion and forms a plexus around the internal carotid artery.
A part of this plexus supplies the dilator pupillae.
Some of these fibres form the deep petrosal nerve for pterygopalatine ganglion;
others give fibres along long ciliary nerve for the ciliary ganglion.
3. The external carotid branches form a plexus around the external carotid artery.
Some of these fibres form the sympathetic roots of the otic and submandibular ganglia.
4. Pharyngeal branches take part in the formation of the pharyngeal plexus.
5. The left superior cervical cardiac branch goes to the superficial cardiac plexus while the right branch goes to the deep cardiac plexus.
Middle Cervical Ganglion
Size & Shape
This ganglion is very small.
Situation
It lies in the lower part of the neck, in front of vertebra C6 just above the inferior thyroid artery, behind
the carotid sheath.
Formation
It is formed by fusion of the fifth and sixth cervical ganglia connections.
It is connected with the inferior cervical ganglion directly, and also through a loop that winds
round the subclavian artery. This loop is called the ansa subclavia.
Branches
1. Grey rami communicans are given to the ventral rami of the 5th and 6th cervical nerves.
2. Thyroid branches accompany the inferior thyroid artery to the thyroid gland. They also supply the parathyroid glands.
3. Tracheal and oesophageal branches.
4. The middle cervical cardiac branch is the largest of the sympathetic cardiac branches. It goes to the deep cardiac plexus.
Inferior Cervical Ganglion
Size & Formation
It is formed by fusion of 7th and 8th cervical ganglia.
This is often fused with the first thoracic ganglion and is then known as the cervicothoracic ganglion or
stellate ganglion because it is star-shaped.
It is situated between the transverse process of vertebra C7 and the neck of the first rib.
It lies behind the vertebral artery, and in front of ramus of spinal nerve C8.
A cervicothoracic ganglion extends in front of the neck of the first rib.
Branches
1. Grey rami communicans are given to the ventral rami of nerves C7 and C8.
2. Vertebral branches form a plexus around the vertebral artery.
3. Subclavian branches form a plexus around the subclavian artery. This plexus is joined by branches
from the ansa subclavia.
4. An inferior cervical cardiac branch goes to the deep cardiac plexus.
Clinical Anatomy:
The head and neck are supplied by sympathetic nerves arising from the upper four thoracic segments of the spinal cord.
Most of these preganglionic fibres pass through the stellate ganglion to relay in the superior cervical ganglion.
Injury to cervical sympathetic trunk produces Horner's syndrome.
It is characterized by:
a. Ptosis - drooping of the upper eyelid.
b. Miosis - constriction of the pupil.
c. Anhydrosis - loss of sweating on that side of the face.
d. Enophthalmos - retraction of the eyeball.
e. Loss of the ciliospinal reflex - pinching the skin on the nape of the neck does not produce dilatation of the pupil (which normally takes place).
Horner's syndrome can also be caused by a lesion within the central nervous system anywhere at or above the first thoracic segment of the spinal cord involving sympathetic fibres.
Watch the lecture on YouTube:










No comments:
Post a Comment